The ACTT-1 study was the first clinical trial in the United States to evaluate treatment for COVID-19. Substantial evidence of efficacy and demonstration of the safety profile led VEKLURY to become the first FDA-approved treatment for COVID-19.4,5
VEKLURY improved clinical outcomes across a spectrum of disease severity in patients hospitalized with COVID-191,2
In the ACTT-1 overall study population, patients experienced

Median 10 days with VEKLURY vs 15 days with placebo; recovery rate ratio: 1.29 (95% CI, 1.12 to 1.49), P < 0.001
- The primary endpoint was time to recovery within 29 days after randomization, based on an 8-point ordinal scale
- Recovery was defined as patients who were no longer hospitalized or hospitalized but no longer required ongoing COVID-19 medical care
ACTT-1 was a randomized, double-blind, placebo-controlled, phase 3 clinical trial in hospitalized adult patients (N=1062) with confirmed SARS-CoV-2 infection and mild, moderate, or severe COVID-19, who received VEKLURY (n=541) or placebo (n=521) for up to 10 days.1

Treatment with VEKLURY was stopped in patients who were discharged from the hospital prior to the completion of 10 days of treatment. Patients in both arms received standard of care.
At baseline in the overall population,2
- 138 patients (13%) did not require supplemental oxygen but required ongoing medical care (COVID-19–related or otherwise)
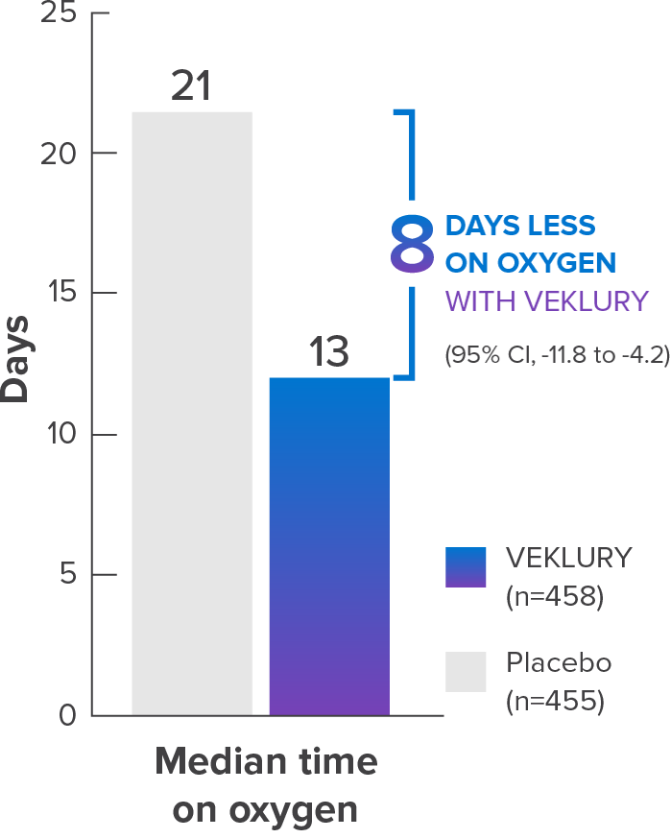
- 435 patients (41%) required supplemental oxygen
- 193 patients (18.2%) required noninvasive ventilation or high-flow oxygen devices
- 285 patients (26.8%) received invasive mechanical ventilation or ECMO
ECMO=extracorporeal membrane oxygenation; R=randomization.
Treatment with VEKLURY earlier in the disease course resulted in the greatest benefit for patients1-3
A prespecified subgroup analysis showed:
- Median time to recovery in patients with symptom onset ≤10 days (n=676) was 9 days with VEKLURY vs 15 days with placebo; recovery rate ratio: 1.37 (95% Cl, 1.14 to 1.64)
- Median time to recovery in patients with symptom onset >10 days (n=383) was 11 days with VEKLURY vs 15 days with placebo; recovery rate ratio: 1.20 (95% Cl, 0.94 to 1.52)
VEKLURY is indicated for patients hospitalized with COVID-19, independent of time from symptom onset
IMPORTANT SAFETY INFORMATION
Contraindication
- VEKLURY is contraindicated in patients with a history of clinically significant hypersensitivity reactions to VEKLURY or any of its components.
Please see additional Important Safety Information below.
VEKLURY helped reduce progression to severe disease, an additional secondary endpoint1-3
VEKLURY reduced incidence of new noninvasive ventilation or high-flow oxygen vs placebo in patients who did not receive either at baseline

VEKLURY reduced incidence of new mechanical ventilation or ECMO vs placebo in patients who did not receive either at baseline

Mortality in overall population1,2
Mortality at Day 29 was a prespecified secondary endpoint
Results in the overall population at Day 29 were not statistically significant.
- The ACTT-1 study was not powered to evaluate a difference in mortality in the overall population


Mortality rates by ordinal scale at Day 29, a post hoc subgroup analysis1-3

- VEKLURY reduced mortality rates at Day 29 in patients on low-flow oxygen at baseline by 70% vs placebo. HR: 0.30 (95% Cl, 0.14 to 0.64)
- No difference was demonstrated in the other baseline oxygen status subgroups
- There was no adjustment to control for multiple testing in this post hoc analysis
Safety parameters in the ACTT-1 study1
Adverse reaction frequency and laboratory abnormalities were comparable between VEKLURY and placebo
Comparable frequency of adverse reactions vs placebo
| Types of adverse reactions | VEKLURY(n=532)n (%) | Placebo(n=516)n (%) |
|---|---|---|
| Any adverse reaction, Grades ≥3 | 41 (8) | 46 (9) |
| Serious adverse reactions | 2 (0.4)* | 3 (0.6) |
| Adverse reactions leading to treatment discontinuation | 11 (2)† | 15 (3) |
*Seizure (n=1), infusion-related reaction (n=1).
†Seizure (n=1), infusion-related reaction (n=1), transaminases increased (n=3), ALT increased and AST increased (n=1), GFR decreased (n=2), acute kidney injury (n=3).
Laboratory abnormalities (Grades 3–4) reported in ≥3% of patients
| Laboratory parameter abnormality‡ | VEKLURY(n=532) | Placebo(n=516) |
|---|---|---|
| ALT increased | 3% | 6% |
| AST increased | 6% | 8% |
| Bilirubin increased | 2% | 5% |
| Creatinine clearance decreased§ | 18% | 20% |
| Creatinine increased | 15% | 16% |
| eGFR decreased | 18% | 24% |
| Glucose increased | 12% | 13% |
| Hemoglobin decreased | 15% | 22% |
| Lymphocytes decreased | 11% | 18% |
| Prothrombin time increased | 9% | 4% |
‡Frequencies are based on treatment-emergent laboratory abnormalities. Graded per Division of AIDS (DAIDS) Table for Grading the Severity of Adult and Pediatric Adverse Events, Version 2.1, dated July 2017.
§Based on the Cockcroft-Gault formula.
| Characteristic | VEKLURY(n=541) | Placebo(n=521) | |
|---|---|---|---|
| Median age ± SD, y | 58.6±14.6 | 59.2±15.4 | |
| Male sex | 65.1% | 63.7% | |
| Race | |||
| White | 51.6% | 55.1% | |
| Black | 20.1% | 22.5% | |
| Asian | 14.6% | 10.7% | |
| Ethnicity: Hispanic/Latinx | 24.8% | 22.3% | |
| Mild/moderate disease* | 10% | 10% | |
| Severe disease† | 90% | 90% | |
| Median time from symptom onset to randomization (IQR), days‡ | 9 (6-12) | 9 (7-13) | |
| Respiratory Status | |||
| Low-flow oxygen | 42.9% | 39.0% | |
| High-flow oxygen | 17.6% | 18.8% | |
| Invasive mechanical ventilation/ECMO | 24.2% | 29.6% | |
| Comorbidities | |||
| Hypertension | 50.6% | 50.9% | |
| Obesity | 45.6% | 45.2% | |
| Type 2 diabetes mellitus | 30.8% | 30.4% | |
*Defined by SpO2 >94% and respiratory rate <24 breaths/minute without supplemental oxygen.
†Defined by a requirement for mechanical ventilation, oxygen requirement, SpO2 ≤94% on room air, or respiratory rate ≥24 breaths/minute.
‡Data on symptom onset were missing for 3 patients.
ECMO=extracorporeal membrane oxygenation; IQR=interquartile range; SpO2=oxygen saturation.
Patient clinical status was assessed on an 8-point ordinal scale with a higher score indicating greater clinical severity.

ECMO=extracorporeal membrane oxygenation.
See clinical outcomes for VEKLURY in high-risk patients
PATIENTS NOT REQUIRING SUPPLEMENTAL OXYGENSee data on VEKLURY and hospital readmissions
REAL-WORLD STUDYImportant Safety Information
Important Safety
Information and Indication
Tap for Important Safety Information, including contraindication for history of clinically significant hypersensitivity to VEKLURY.
VEKLURY is indicated for the treatment of COVID-19 in adults and pediatric patients (birth to <18 years of age weighing ≥1.5 kg), who are hospitalized, or not hospitalized, with mild-to-moderate COVID-19 and are at high risk for progression to severe COVID-19, including hospitalization or death.
Contraindication
- VEKLURY is contraindicated in patients with a history of clinically significant hypersensitivity reactions to VEKLURY or any of its components.
Warnings and precautions
- Hypersensitivity, including infusion-related and anaphylactic reactions: Hypersensitivity, including infusion-related and anaphylactic reactions, has been observed during and following administration of VEKLURY; most reactions occurred within 1 hour. Monitor patients during infusion and observe for at least 1 hour after infusion is complete for signs and symptoms of hypersensitivity as clinically appropriate. Symptoms may include hypotension, hypertension, tachycardia, bradycardia, hypoxia, fever, dyspnea, wheezing, angioedema, rash, nausea, diaphoresis, and shivering. Slower infusion rates (maximum infusion time of up to 120 minutes) can potentially prevent these reactions. If a severe infusion-related hypersensitivity reaction occurs, immediately discontinue VEKLURY and initiate appropriate treatment (see Contraindications).
- Increased risk of transaminase elevations: Transaminase elevations have been observed in healthy volunteers and in patients with COVID-19 who received VEKLURY; these elevations have also been reported as a clinical feature of COVID-19. Perform hepatic laboratory testing in all patients (see Dosage and administration). Consider discontinuing VEKLURY if ALT levels increase to >10x ULN. Discontinue VEKLURY if ALT elevation is accompanied by signs or symptoms of liver inflammation.
- Risk of reduced antiviral activity when coadministered with chloroquine or hydroxychloroquine: Coadministration of VEKLURY with chloroquine phosphate or hydroxychloroquine sulfate is not recommended based on data from cell culture experiments, demonstrating potential antagonism, which may lead to a decrease in the antiviral activity of VEKLURY.
Adverse reactions
- The most common adverse reaction (≥5% all grades) was nausea.
- The most common lab abnormalities (≥5% all grades) were increases in ALT and AST.
Dosage and administration
- Administration should take place under conditions where management of severe hypersensitivity reactions, such as anaphylaxis, is possible.
- Treatment duration:
- For patients who are hospitalized, VEKLURY should be initiated as soon as possible after diagnosis of symptomatic COVID-19.
- For patients who are hospitalized and do not require invasive mechanical ventilation and/or ECMO, the recommended treatment duration is 5 days. If a patient does not demonstrate clinical improvement, treatment may be extended up to 5 additional days, for a total treatment duration of up to 10 days.
- For patients who are hospitalized and require invasive mechanical ventilation and/or ECMO, the recommended total treatment duration is 10 days.
- For patients who are not hospitalized, diagnosed with mild-to-moderate COVID-19, and are at high risk for progression to severe COVID-19, including hospitalization or death, the recommended total treatment duration is 3 days. VEKLURY should be initiated as soon as possible after diagnosis of symptomatic COVID-19 and within 7 days of symptom onset for outpatient use.
- Testing prior to and during treatment: Perform hepatic laboratory and prothrombin time testing prior to initiating VEKLURY and during use as clinically appropriate.
- Renal impairment: No dosage adjustment of VEKLURY is recommended in patients with any degree of renal impairment, including patients on dialysis. VEKLURY may be administered without regard to the timing of dialysis.
Pregnancy and lactation
- Pregnancy: Available clinical trial data for VEKLURY in pregnant women have not identified a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes following second- and third-trimester exposure. There are insufficient data to evaluate the risk of VEKLURY exposure during the first trimester. Maternal and fetal risks are associated with untreated COVID-19 in pregnancy.
- Lactation: VEKLURY can pass into breast milk. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for VEKLURY and any potential adverse effects on the breastfed child from VEKLURY or from an underlying maternal condition. Breastfeeding individuals with COVID-19 should follow practices according to clinical guidelines to avoid exposing the infant to COVID-19.
Indication
VEKLURY is indicated for the treatment of COVID-19 in adults and pediatric patients (birth to <18 years of age weighing ≥1.5 kg), who are hospitalized, or not hospitalized, with mild-to-moderate COVID-19 and are at high risk for progression to severe COVID-19, including hospitalization or death.
Please see full Prescribing Information for VEKLURY.
ECMO=extracorporeal membrane oxygenation; HR=hazard ratio.